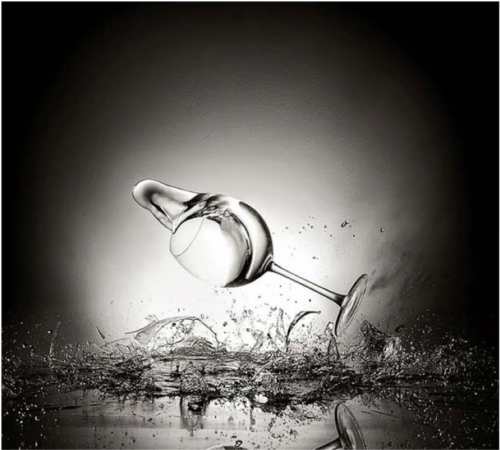
Falls Steal Dreams
If you fall, I’ll be there…
-Floor
Falls Steal Dreams
Some time ago I heard one of the most memorable statements ever made on the topic of falling. Louis Tenenbaum, an expert in the area ofaging in place, delivered it during a webinar. He said: “falls steal dreams.”
See
